Ensure education for recognizing/reporting suspicious behaviors
Reprinted with permission from New Perspectives, Journal of the Association of Healthcare Internal Auditors, Inc. Volume 41/Number 5.
By Jennifer Splawski, PharmD, MS, BCPS
What to do if you suspect drug diversion
Controlled substance medication diversion is on the rise in healthcare. Reports indicate that diversion costs the healthcare industry more than $70 billion per year, and up to 10 percent of healthcare providers will divert drugs at some point in their careers.
However, most provider personnel do not receive adequate training to prevent and report drug diversion. Does your team know what to do if they suspect diversion at your facility?
Barriers to reporting drug diversion
Often management and staff are unaware of the actions to take when diversion is suspected and reported. When surveyed, 50 percent of hospital respondents reported that they did not have a procedure, or did not know, what they would do when they identified a possible drug diverter.
Additionally, provider personnel commonly believe that diversion would not happen in their unit due to close working relationships and trust among colleagues. Individuals may also be unable to recognize signs and symptoms of drug diversion or drug abuse. Someone diverting medications may put off inquiries by saying their behavior is due to being stressed, having a bad day, or being burned out and tired.
Another barrier to drug diversion reporting is the fear of reporting on a colleague. This includes fear of retaliation for reporting diversion suspicions from staff members or management. Feeling apprehensive when reporting a superior is understandable, such as when a certified registered nurse anesthetist reports an anesthesiologist or a pharmacy technician reports a pharmacist.
Finally, a potential reporter of drug diversion may be worried about being a part of a lawsuit or a diversion case that could affect the reporter’s professional license. Despite the fears, everyone should know that reporting can potentially save a patient’s or even an employee’s life.
The DEA recognizes five classes of drugs that are frequently misused—anabolic steroids, central nervous system depressants, hallucinogens, opioids, and stimulants. The medications can be diverted for use in recreational purposes, relief of addiction or withdrawal, monetary gain, self-medication for pain, anxiety, or sleep.
You need to be prepared to answer common questions regarding drug diversion reporting and be able to recommend tools for frontline line healthcare providers to understand, identify, and report behaviors that may affect patient and employee safety.
The consequences of drug diversion by role
Drug diversion has consequences that can affect everyone from the patient to the entire health system.
Diverters − Individuals who are diverting medications can be subject to civil or criminal penalties. They could possibly forfeit licensure, suffer career damage, or die. In addition, if diverters survive an overdose, they could suffer an anoxic brain injury or acquire an infection from an unsanitary injection.
Coworkers − The coworkers of drug diverters can suffer consequences from diversion schemes. Coworkers may unknowingly aid diversion by witnessing fake wasting or disposal by coworkers who are diverting medications. Coworkers can also risk physical harm if the diverters leave
contaminated needles or broken vials in nursing units and other patient care areas.
Organizations − The individual’s employer and health system also suffer the consequences of drug diversion. Employers can be affected by a loss of revenue from missing medications, increased employee absenteeism, and increased resources devoted to investigation and testing. Regulators can impose large fines and drug diversion lawsuits can result in substantial monetary settlements. One health system paid $7.75 million to the DEA to settle allegations of inappropriate pharmacy operations that included diversion.
Patients − Patients are the parties most affected by drug diversion. The healthcare provider’s oath is to “do no harm.” When patients are being treated by individuals who are diverting medications, they very possibly receive substandard care. Patients may not get appropriate pain medication after a procedure, or they may be infected by a contaminated or adulterated drug. They can become sicker than when they came into the hospital.
Drug diversion has a large effect across the healthcare industry. Reporting of any potential drug diversion is extremely important. An anonymous report can save lives and avoid other serious consequences.
Signs of impairment, substance misuse, and diversion
Staff cannot always easily recognize changes in colleagues’ behavior regarding substance misuse or drug diversion. When a colleague looks to be impaired, they are not necessarily diverting medications. If a colleague is diverting medications, they are not necessarily impaired.
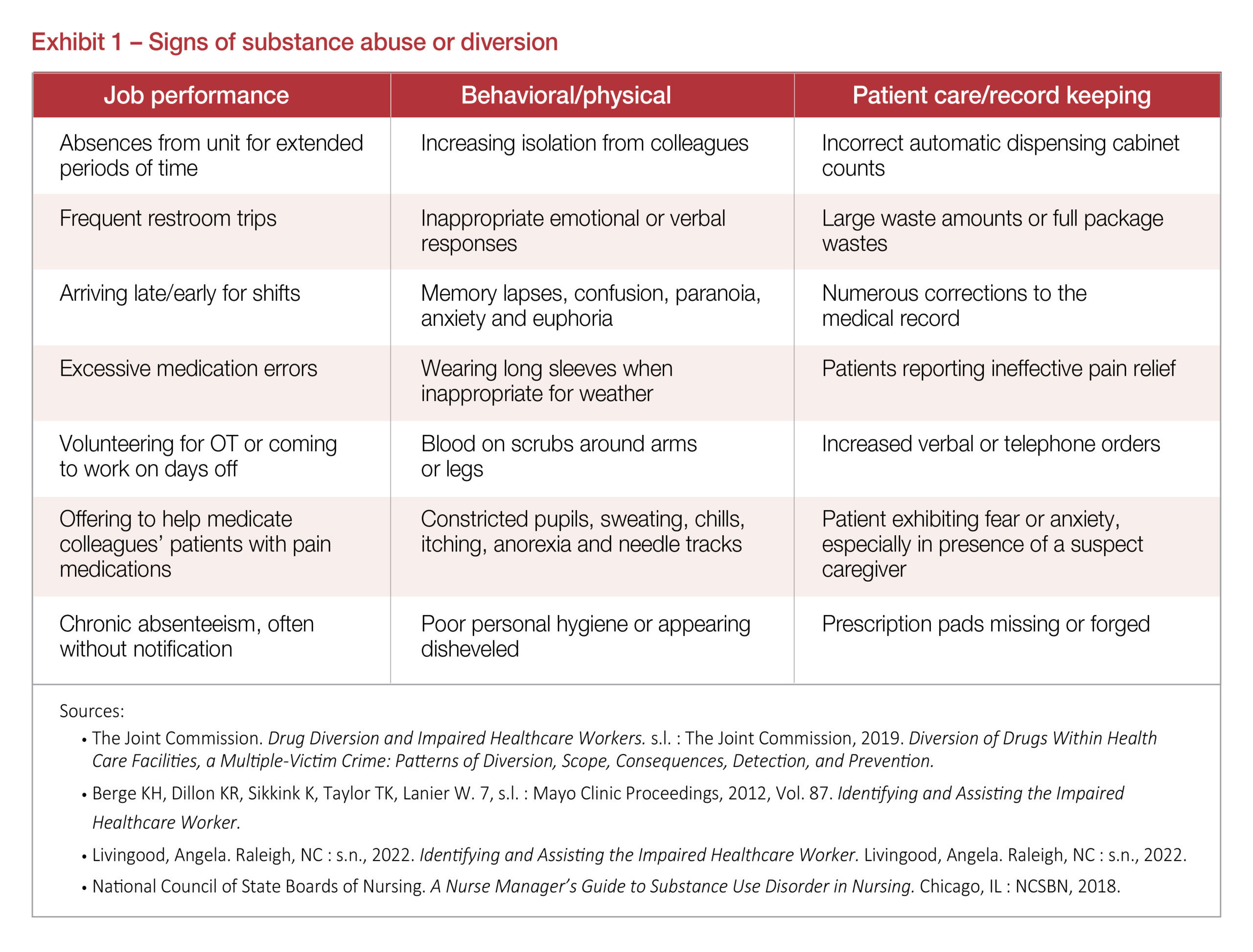
Diversion-related changes in behavior can be subtle and hard to differentiate from normal stress-related behaviors and substance misuse. Exhibit 1 provides a reference on how a colleague can change if they struggle with substance abuse. The summary is not inclusive of all possible attributable behaviors. Staff need to be reminded that if they see something, they should say something. Failing to report a concern can harm patients or place a colleague’s life at risk.
Steps to promote a culture of safety around diversion reporting
Promoting a culture of safety is key to diversion prevention. All hospital employees, not just direct patient caregivers, need to be educated about diversion and what to do if they identify a potential risk for diversion. For example, what if a housekeeping employee finds a half-used vial of a controlled substance in a breakroom while they are cleaning?
Implement policies and procedures
Each employee type should have training customized to how their work can be affected by drug diversion and should have the tools to report incidents. Policies should be readily available for employees to reference, updated routinely, and include a minimum annual education expectation regarding policy refreshers and updates. When healthcare workers understand why policies and procedures exist and buy into a culture of safety, diversion can be detected earlier and have better outcomes.
Establish reporting mechanisms
The DEA takes the position that employees have the responsibility to report knowledge of drug diversion to their employer because drug diversion can pose a substantial public health risk and should be taken seriously. Your organization should keep reports confidential and take reasonable steps to maintain the confidentiality of the individual who reports suspected diversion.
Your organization should also:
- Encourage reporting from all staff members. Employees should not fear reporting or suffer retaliation.
- Have methods for reporting suspected diversion, such as a confidential hotline, email address and/or an online reporting portal.
- Ensure that your employees are educated about how and where to report these events.
- Educate your employees to report these events through dedicated channels or to security or management, and to never confront the suspected employee on their own.
Provide resources for drug diverters to get help
Healthcare organizations should offer employees treatment instead of termination and provide resources to care for employees suffering from substance use disorder. Facilitating treatment for impaired employees is more cost-effective than replacing them.
Healthcare workers may be reluctant to admit they have a problem due to stigma and fear of losing their jobs or licenses. According to the National Council of State Boards of Nursing, many states offer treatment and rehabilitation programs instead of disciplinary action. The programs will remove a nurse from patient care until recovery has been completed and they are safe to return to practice. Upon returning to practice, the individual and the employer should then decide if the individual should return to work in his/her previous scope or should no longer handle controlled substances.
Organizations should recognize the employee’s right to be accommodated when they have a diagnosed substance use disorder. Recognition does not mean a preferred or ideal accommodation, but one that works for both the employee and the employer. Below are some resources for substance use disorder treatment and recovery.
Resources for substance use disorder treatment and recovery
- Seeking Drug Abuse Treatment: Know What to Ask (https://nida.nih.gov/sites/default/files/treatmentbrochure_web.pdf)
- SAMHSA’s National Helpline is a free, confidential, 24/7, 365 days a year treatment referral and information service, call 800-662-4357
(https://www.samhsa.gov/) - National Suicide Prevention Lifeline, 24/7,365 days a year, call 800-273-8255 (https://suicidepreventionlifeline.org/)
Hospitals have a duty to make drug diversion reporting accessible
Healthcare providers have easy access to prescription medications and diversion of these medications can lead to severe patient harm. Hospitals and other healthcare organizations have a responsibility to make sure that everyone knows what to do if they suspect drug diverson. The best way to do that is to provide answers to commonly asked questions about drug diversion reporting, ensure that sound policies and procedures exist, and verify that education has been provided.
Healthcare providers must feel empowered to say something if they see something. Speaking up could save a patient or colleague’s life. Everyone is responsible for making sure patients and colleagues are free from harm.
Resources
TJC – Quick Safety Issue 48: Drug Diversion and Impaired Health Care Workers (https://www.jointcommission.org/resources/newsandmultimedia/newsletters/newsletters/quick-safety/quick-safety-48-drug-diversion-andimpairedhealth-care-workers/)
- What Is a Prescriber’s Role in Preventing the Diversion of Prescription Drugs? (https://www.cms.gov/files/document/prescriberroledrugdiversion033115pdf#:~:text=Drug%20diversion%20is%20the%20illegal,and%20ultimately%20to%20the%20patient)
- A Nurse Manager’s Guide to Substance Use Disorder in Nursing (https://www.ncsbn.org/3692.htm)
- Signs and Behaviors of Impaired Colleagues (https://www.aana.com/practice/health-and-wellness-peer-assistance/About-AANA-Peer-Assistance/substanceuse-disorder-workplace-resources/signs-andbehavior-of-impaired-colleagues)