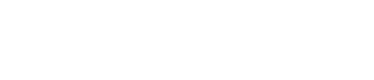
Drug shortages continue to strain hospital operations, budgets, and clinical teams. With 75% of pharmacy leaders citing shortages as their most urgent challenge and shortage-related labor costs approaching $900M each year, multi-hospital systems need stronger system-level coordination.
Rising national drug spending, which increased by 11.4% in 2024, adds even more pressure on leaders to move from isolated, site-specific tactics to unified shortage response.
For large health systems, rebalancing inventory across hospitals is one of the most effective ways to protect patient care during volatile supply conditions. A unified, predictive approach transforms reactive “fire drills” into coordinated system-level action.
Step 1: Get the Right Data in Place Before Redistributing Inventory
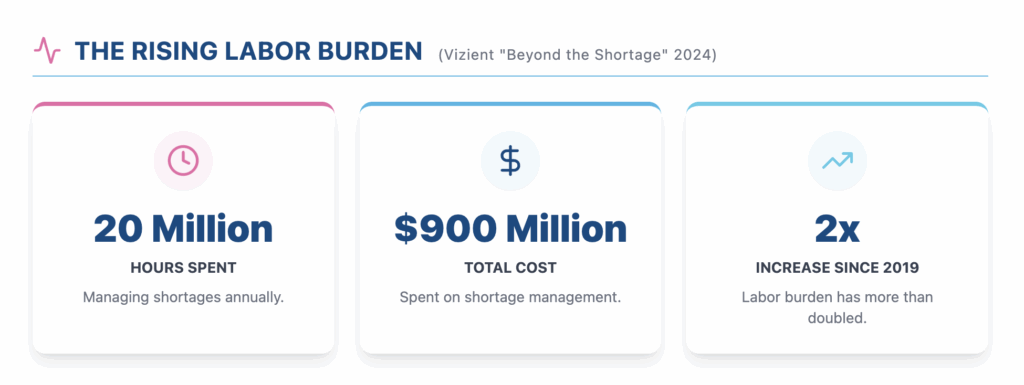
System-level redistribution requires a complete and accurate picture of supply and demand across every facility. The right data ensures decisions are grounded in real risk rather than assumptions or incomplete reporting.
Inventory on Hand (IOH)
IOH establishes a clear view of how supply is distributed across the system. It highlights concentrated stock, emerging shortages, and surplus inventory that could support hospitals with greater need. Reliable IOH is the foundation for any redistribution effort.
Days on Hand (DOH)
DOH measures how long each hospital’s inventory will last under typical utilization. It normalizes comparisons across hospitals of different sizes and complexity and helps leaders prioritize movement based on depletion risk rather than volume alone.
Usage Trends and Demand Variability
Hospitals within a system experience different acuity patterns and clinical demands. Understanding consumption trends helps avoid removing supply from facilities that may face sudden surges. This insight supports more stable and predictable redistribution.
Predictive Shortage Indicators
Teams need early visibility into drugs that are trending toward shortage so they can act before patient care is affected. ShortageCheck strengthens this visibility by surfacing emerging risks up to 90 days lead time, with an average lead time of 52 days, and ranking the products most likely to impact hospital operations. With shortage workload more than doubling in recent years, early warning signals are essential.
Financial Impact and Contract Visibility
Hospitals can see cost increases of up to 20 percent during shortages, making it essential to understand contract positioning, price implications, and system-level spend before moving inventory. CostCheck provides this critical financial visibility by analyzing pricing variations across facilities, contract terms, and potential alternative products. This approach prevents inventory movements from inadvertently triggering higher costs, compromising contact compliance, and supports stability in a year when national drug spending climbed $50B.
Step 2: Establish Governance for Fast, System-Level Decisions
Effective rebalancing depends on governance that enables quick, consistent decisions across the system. Start by defining who can authorize redistribution, substitution, and allocation changes so action does not stall when supply tightens.
Then, align on system-wide clinical prioritization criteria to ensure that the highest-need patient populations and units receive supply first. Escalation triggers anchored in DOH thresholds and predictive alerts help teams intervene at the right time.
Finally, establish standardized communication expectations and implement a centralized shortage playbook to keep pharmacy, clinical, and supply-chain teams coordinated when conditions escalate and workload intensifies.
Step 3: Execute Redistribution with Operational Guardrails
With data and governance in place, health systems can move inventory safely and efficiently.
First, IOH, DOH, and utilization data identify which sites can lend supply without compromising their own readiness and which require immediate support. Clinical teams verify appropriateness before every transfer to ensure therapeutic consistency and patient safety.
Next, allocation criteria based on acuity, utilization, and service-line needs keep decisions equitable. A defined approval workflow prevents delays and maintains continuity of care during rapid shifts in supply.
Throughout the process, chain-of-custody standards protect safety and compliance during transfers between hospitals. Clear communication across pharmacy, nursing, and clinical operations ensures each redistribution aligns with care delivery needs.
To streamline this entire process, ShortageCheck supports coordinated execution by prioritizing shortages by risk, aligning teams across sites, and simplifying communication during high-pressure situations.
Step 4: Recognize When Rebalancing Is Not Enough and Plan for What Comes Next
Redistribution has limits. When system-wide DOH declines, when predictive alerts signal sustained national constraints, or when alternatives narrow, leaders must transition from internal shifts to broader mitigation strategies.
Therapeutic and clinical committees may need to activate substitutions and update dispensing workflows, order sets, and documentation. Systems benefit from shifting toward fully predictive mitigation, supported by ShortageCheck’s ability to forecast and prioritize shortages so teams can stabilize supply before issues escalate.
Health systems that rebalance inventory with strong data, consistent governance, and clear operational guardrails can stay ahead of fast-moving shortages. This coordinated approach protects patient care, reduces emergency purchasing, and strengthens readiness for whatever the national supply environment brings next.